By Victoria Colliver

Jennifer Mitchell, PhD (left), professor of neurology and psychiatry and behavioral sciences with Sydney Griffith (right), clinical research coordinator. [Photo: Noah Berger]
In the 47 years since she was raped by multiple assailants in San Francisco’s Chinatown, Susie Chin has worked to heal the fear and shame in her mind through traditional therapy. But the body never forgets.
“I felt like I had a good handle on everything conceptually and intellectually, but the physical senses from the trauma were still in my body,” said Chin, who is now 63. “I could ‘muscle through’ certain feelings but, in other areas, my body didn’t seem to get the memo. It was exhausting to be so hyper-vigilant to danger. My startle reflex was so intense that if someone surprised me with a tap on the shoulder, I’d inadvertently jump out of my skin and scare that person right back”
She realized only recently that her symptoms were post-traumatic stress disorder (PTSD), and learned through research how MDMA – known in street parlance as Ecstasy or Molly – was being used to treat people who were suffering from it.
After consulting a trusted mental health professional familiar with MDMA’s use in people with trauma, Chin felt comfortable enough to enroll in a late-stage clinical trial through UC San Francisco to test the efficacy and safety of MDMA, short for 3,4-methylenedioxymethamphetamine, in conjunction with therapy for the treatment of patients with severe-to-moderate PTSD.
For Chin, the entire process – from the therapy before the monitored MDMA-assisted sessions to the follow-ups – were helpful. “I never felt like I was ‘on a trip’ or out of control,” she said. “I felt less inhibited, more open, sensitive and more attuned to what I was feeling.”
High marks in trial results
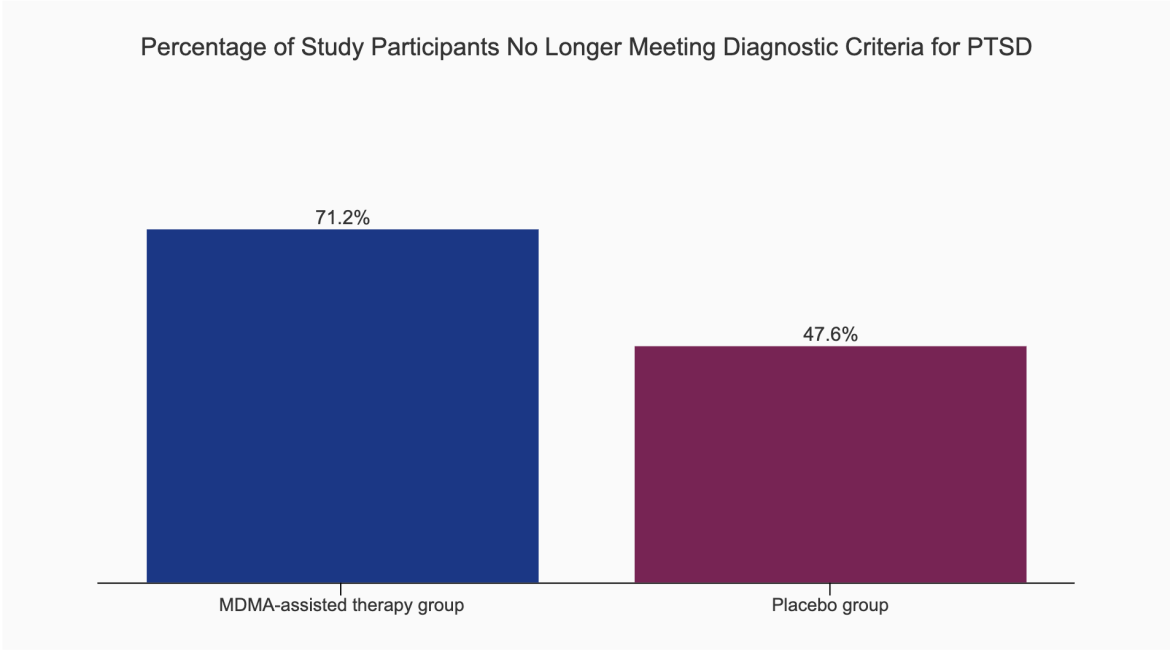
Chin was among 104 participants in the multi-site trial, which found that those suffering from moderate or severe PTSD who took MDMA, paired with psychotherapy sessions, were about twice as likely to recover from their trauma as those who took a placebo.
The findings, published Sept. 13, 2023, in the journal Nature Medicine, demonstrate the illegal so-called party drug could be a powerful new tool in treating people with moderate-to-severe PTSD.
The trial, which included a diverse pool of participants, validates an earlier Phase 3 study and is the final step in clinical drug testing. This puts MDMA, used in conjunction with therapy to treat PTSD, on track to be the first psychedelic to seek approval from the U.S. Food and Drug Administration.
By the end of the 18-week trial period, 71.2% of the people in the MDMA-assisted therapy group no longer met the diagnostic criteria for PTSD, versus 47.6% of those in the therapy-plus-placebo group. MDMA produced no serious, adverse side effects.
The trial’s sponsor and funder, the private biopharmaceutical company MAPS Public Benefit Corp., plans to submit its drug application to the FDA this year and hopes for FDA approval by the end of 2024.
“These data are the culmination of several decades worth of research that demonstrate the effectiveness of MDMA-assisted therapy for PTSD. We are nearing the tipping point in establishing the benefits of psychedelic therapy for mental health conditions,” said the paper’s first author, Jennifer Mitchell, PhD, professor of neurology and of psychiatry and behavioral sciences and a member of the Weill Institute for Neurosciences at UCSF. Mitchell was also the first author of the paper that published the results from the first clinical trial.
How the “love drug” works to rewire the brain
What gets Mitchell and other researchers excited about this therapy is that it doesn’t just mask or blunt the symptoms of trauma. It appears to change the brain in a way that allows people to feel more compassionate toward themselves, and that helps make therapy more accessible and effective.
The drug, which earned the name Ecstasy for its ability to enhance empathy and closeness, stimulates the release of a neurotransmitter known as serotonin, which helps regulate mood. That in turn releases oxytocin, a neuromodulator that’s released by the pituitary gland, which is important for feelings of closeness and communication.
“MDMA can allow you to process deep-seated trauma by enabling the transformation of fear memories in a part of the brain called the amygdala in a manner that doesn’t make you withdraw or detach out of shame or fear, but instead helps you to accept and heal,” Mitchell explained.
That same bonding power that makes MDMA effective in treatment is what turned it into a party drug and a rave scene favorite in the 1980s. This prompted the DEA to declare an emergency ban on the drug in 1985 and to put it on the list of Schedule I substances, the same category as heroin and LSD.
Schedule I drugs are considered to have no currently acceptable medical use, and a high potential for abuse. Researchers can only study them under strict protocols with special approval from the FDA.
MDMA was developed in 1912 by the German pharmaceutical giant Merck as a blood-clotting agent. The drug all but languished until the 1970s, when it was rediscovered by Berkeley-born chemist Alexander Shulgin. Shulgin tested the compound on himself and others, including a psychologist who used it in conjunction with therapy.
A drug regimen that also includes therapy
Susie Chin, study participant
Amy Emerson, chief executive officer of MAPS PBC, the trial sponsor, said this will be the first time the FDA has been asked to approve a drug that also requires psychotherapy.
If it is approved by the FDA, the DEA would still need to move the drug from the most restrictive category, known as Schedule I, to a less restrictive level that would allow it to be used therapeutically.
“Given the urgent need for novel effective treatment options for PTSD, and with consistent results from two positive Phase 3 studies, we are hopeful that MDMA-assisted therapy, if approved by the FDA, could be a new option for patients, providers and therapists to consider,” she said.
Chin said being in the study helped her to heal the horrific sexual assault, along with traumatic experiences dating back to childhood. The therapy staff earned her trust, and the trial’s association with UCSF gave it legitimacy.
“Was it a miracle cure, and all my symptoms are now gone? No,” Chin said, adding she could have benefited from additional sessions. “But I feel more comfortable, generally. I’m less tense, less anxious. I have more self-compassion and a better sense of agency so I can take action toward achieving what I want in life.”
Read the study
- Nature Medicine: MDMA-assisted therapy for moderate to severe PTSD: a randomized, placebo-controlled phase 3 trial
About UCSF Psychiatry and Behavioral Sciences
The UCSF Department of Psychiatry and Behavioral Sciences and the Langley Porter Psychiatric Institute are among the nation's foremost resources in the fields of child, adolescent, adult, and geriatric mental health. Together they constitute one of the largest departments in the UCSF School of Medicine and the UCSF Weill Institute for Neurosciences, with a mission focused on research (basic, translational, clinical), teaching, patient care, and public service.
UCSF Psychiatry and Behavioral Sciences conducts its clinical, educational, and research efforts at a variety of locations in Northern California, including the UCSF Nancy Friend Pritzker Psychiatry Building; UCSF Langley Porter Psychiatric Hospital; UCSF Medical Centers at Parnassus Heights, Mission Bay, and Mount Zion; UCSF Benioff Children’s Hospitals in San Francisco and Oakland; Zuckerberg San Francisco General Hospital and Trauma Center; the San Francisco VA Health Care System; UCSF Fresno; and numerous community-based sites around the San Francisco Bay Area.
About the UCSF Weill Institute for Neurosciences
The UCSF Weill Institute for Neurosciences, established by the extraordinary generosity of Joan and Sanford I. "Sandy" Weill, brings together world-class researchers with top-ranked physicians to solve some of the most complex challenges in the human brain.
The UCSF Weill Institute leverages UCSF’s unrivaled bench-to-bedside excellence in the neurosciences. It unites three UCSF departments—Psychiatry and Behavioral Sciences, Neurology, and Neurological Surgery—that are highly esteemed for both patient care and research, as well as the Neuroscience Graduate Program, a cross-disciplinary alliance of nearly 100 UCSF faculty members from 15 basic-science departments, as well as the UCSF Institute for Neurodegenerative Diseases, a multidisciplinary research center focused on finding effective treatments for Alzheimer’s disease, frontotemporal dementia, Parkinson’s disease, and other neurodegenerative disorders.
About UCSF
The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. UCSF Health, which serves as UCSF’s primary academic medical center, includes top-ranked specialty hospitals and other clinical programs, and has affiliations throughout the Bay Area.