By Jan Greene

People with HIV were more likely to report suicidal thoughts if they had been diagnosed with depression or anxiety, misused stimulants, or reported use of multiple substances, according to new research from UC San Francisco and Kaiser Permanente, published in the Journal of Affective Disorders.

Derek Satre, PhD
The results could provide useful information to health care providers treating people with HIV, said lead author Derek Satre, PhD, a professor in the UCSF Department of Psychiatry and Behavioral Sciences and adjunct investigator with the Kaiser Permanente Division of Research.
“People with HIV have higher rates of depression, anxiety, and other medical conditions than people without HIV,” Satre said. “They also have higher rates of substance use that put them at risk for suicidal behavior. While we knew about these vulnerabilities, this study provides health care teams with specific risk factors they can keep in mind to better identify patients who may be at risk for suicidal thoughts.”
The study included 2,829 people with HIV who were screened for substance use and depression between October 2018 and July 2020 at three Kaiser Permanente primary care clinics in Northern California. The study population was 82% male, 56% white, with an average age of 54. The average length of time since known HIV infection was 18 years.
Substance use-related risk findings.
The researchers analyzed screening results along with information from patient medical records on psychiatric diagnoses; HIV treatments and control; insurance coverage; and neighborhood economic conditions.
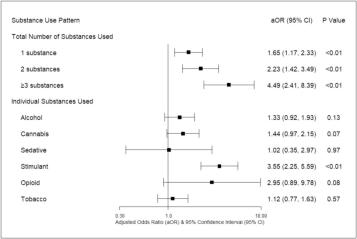
They found that suicidal ideation was higher among those reporting substance use, particularly among those using stimulants (such as methamphetamine or cocaine) or multiple substances. Compared with those who did not report any substance use problems, odds of suicidal thoughts were 1.7 times higher with use of 1 substance, and 4.5 times higher with 3 or more substances.
Overall, 60% reported no problem with substance use, 27% reported using 1 substance, 10% reported using 2 substances, and 3% reported using 3 or more substances.
The patients with HIV and a diagnosis of depression or anxiety were also at greater risk for suicidal thoughts, with 4.2 times higher odds of suicidal thoughts with depression, compared with those without depression. Overall, 16% of the group had a depression diagnosis and 16% had an anxiety disorder diagnosis.
“These findings reinforce the importance of treatment for these prevalent psychiatric disorders among people with HIV to reduce risk of suicidal behavior,” Satre said.
Screening in primary care
Patients included in this analysis were part of the Promoting Access to Care Engagement (PACE) study, which evaluated primary care-based electronic screening for substance use, depression, and anxiety symptoms among people with HIV. Participants were asked to complete a self-administered questionnaire before their primary care visit. The questionnaire included the Tobacco, Alcohol, Prescription medication, and other Substance use (TAPS) instrument, along with the Patient Health Questionnaire (PHQ-9).
Item 9 on the PHQ-9 questionnaire asks about the frequency over the previous 2 weeks of “thoughts that you would be better off dead, or of hurting yourself.”
As part of the PACE study, an alert was added to the electronic health record (EHR) when the screening identified suicidal thoughts in a patient. “Having those results integrated into the EHR with automated identification of patients who endorsed suicidal ideation was very well received by providers, who were able to quickly follow up with patients when clinically necessary,” senior study author Michael Silverberg, PhD, MPH, a research scientist and associate director with the Kaiser Permanente Division of Research.
Overall, 8% of patients reported suicidal thoughts, which is higher than what is usually seen in the general population without HIV, but lower than what some other studies of people with HIV have found. The lower rate in this study population could be because these patients have health insurance coverage and also because most maintain regular primary care visits, and have their HIV under control, the authors said.
The analysis also supported the use of a standardized, computerized screening process for patients with HIV being seen in primary care, Silverberg said. “Given the vulnerability of this population, screening for suicidal ideation and factors associated with suicide risk should be a routine component of clinical care for people with HIV, although there are certainly challenges with implementing screening in primary care settings,” he said.

Michael Silverberg, PhD, MPH
The study also found higher likelihood of suicidal ideation among those with Medicaid as a health insurance source. “Our finding that people with public insurance are at greater risk may be an indicator of socioeconomic vulnerability in some of our patients,” Satre said.
The analysis did not find a connection between suicidal thoughts and HIV-related measures such as viral control, nor an effect of neighborhood economic conditions.
The study was funded by the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and the UCSF Dolby Family Center for Mood Disorders.
Additional co-authors were Stacy A. Sterling, DrPH, MSW, Varada Sarovar, PhD, Tory Levine, MPH, Amy S. Leibowitz, PsyD, and Alexandra N. Lea, MPH, of the Division of Research; Kathryn Ridout, MD, C. Bradley Hare, MD, Mitchell N. Luu, MD, Jason Flamm, MD, of The Permanente Medical Group; James W. Dilley, MD, of UCSF; and Thibaut Davy-Mendez, PhD, of the University of North Carolina at Chapel Hill.
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow them @KPDOR.
About UCSF Psychiatry and Behavioral Sciences
The UCSF Department of Psychiatry and Behavioral Sciences and the Langley Porter Psychiatric Institute are among the nation's foremost resources in the fields of child, adolescent, adult, and geriatric mental health. Together they constitute one of the largest departments in the UCSF School of Medicine and the UCSF Weill Institute for Neurosciences, with a mission focused on research (basic, translational, clinical), teaching, patient care, and public service.
UCSF Psychiatry and Behavioral Sciences conducts its clinical, educational, and research efforts at a variety of locations in Northern California, including the UCSF Nancy Friend Pritzker Psychiatry Building; UCSF Langley Porter Psychiatric Hospital; UCSF Medical Centers at Parnassus Heights, Mission Bay, and Mount Zion; UCSF Benioff Children’s Hospitals in San Francisco and Oakland; Zuckerberg San Francisco General Hospital and Trauma Center; the San Francisco VA Health Care System; UCSF Fresno; and numerous community-based sites around the San Francisco Bay Area.
About the UCSF Weill Institute for Neurosciences
The UCSF Weill Institute for Neurosciences, established by the extraordinary generosity of Joan and Sanford I. "Sandy" Weill, brings together world-class researchers with top-ranked physicians to solve some of the most complex challenges in the human brain.
The UCSF Weill Institute leverages UCSF’s unrivaled bench-to-bedside excellence in the neurosciences. It unites three UCSF departments—Psychiatry and Behavioral Sciences, Neurology, and Neurological Surgery—that are highly esteemed for both patient care and research, as well as the Neuroscience Graduate Program, a cross-disciplinary alliance of nearly 100 UCSF faculty members from 15 basic-science departments, as well as the UCSF Institute for Neurodegenerative Diseases, a multidisciplinary research center focused on finding effective treatments for Alzheimer’s disease, frontotemporal dementia, Parkinson’s disease, and other neurodegenerative disorders.
About UCSF
The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. UCSF Health, which serves as UCSF’s primary academic medical center, includes top-ranked specialty hospitals and other clinical programs, and has affiliations throughout the Bay Area.