By Levi Gadye
The ideal therapy for a disease works exclusively at the site of the disease.
But when it comes to the brain, which is wrapped in a protective barrier and contains thousands of different cell types, this ideal is very hard to achieve.
Now, a group of scientists at UC San Francisco—which includes Department of Psychiatry and Behavioral Sciences faculty member Anna Victoria Molofsky, MD, PhD—have been awarded more than $30 million by the Advanced Research Projects Agency for Health (ARPA-H) to lead the Cell Therapies for Neuroinflammation and Neurodegeneration (CT-NEURO) project, which will develop a new technology dubbed “tissue GPS.” The system uses engineered T cells to guide therapies directly to their targets in the brain to treat neurological diseases, like the deadly brain cancer glioblastoma, multiple sclerosis and Alzheimer’s.
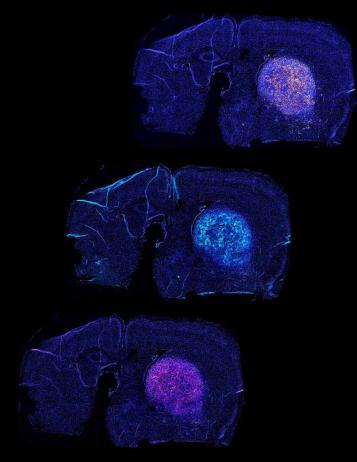
The “tissue GPS” system enables engineered T-cells to deliver disease therapies to specific regions in the brain. In an early experiment, these engineered T-cells (cyan) successfully found and treated a glioblastoma (yellow) in laboratory mice. Dying tumor cells are shown in magenta, bottom. [Image: Payal Watchmaker/UCSF]
These immune cells navigate by detecting molecular markers called antigens that appear on the surface of target cells like street addresses, replete with nine-digit zip codes. They only transfer their payload of anti-inflammatories or cancer-killing molecules once they have arrived at the right location.
The tissue GPS system may give immune cells the ability to pass through molecular gates in the blood brain barrier; find and stick to target cells; and safely deliver a tailored therapy. With such an exacting approach, the hope is that patients will be spared many of the uncomfortable or even dangerous side effects associated with other therapies.
“The field has many molecular tools that could potentially address conditions like neuroinflammation or Alzheimers, but it is challenging to know how to use these tools in a way that would precisely target the brain,” said Wendell Lim, PhD, project lead, UCSF Byers Distinguished Professor of Cellular and Molecular Pharmacology, and director of the UCSF Cell Design Institute. “Tissue GPS will ensure that therapies have a maximal effect in the right parts of the brain, making it much easier to treat complex disease.”
Disbursed over five years, the funds will support Molofsky, Lim, and UCSF colleagues Scott Zamvil, MD, PhD; Hideho Okada, MD, PhD; and Dean Sheppard, MD, in developing the system.
The UCSF researchers will test the system’s delivery of therapies for brain tumors; neuroinflammation; demyelination (the loss of insulation on neural wires, like in multiple sclerosis); and neurodegeneration. They also will test its ability to reach other specific organs, like the lungs.
The team has mapped out antigens that are present throughout the brain, as well as the molecular sensors required for the tissue GPS to navigate to various brain regions. In an early experiment, their approach enabled engineered T-cells to treat brain tumors in mice.
“Immune cells are incredibly adept at traversing the body to reach a target,” Lim said. “These living cells could provide a powerful way to get therapies to where they need to be.”
About UCSF Psychiatry and Behavioral Sciences
The UCSF Department of Psychiatry and Behavioral Sciences and the Langley Porter Psychiatric Institute are among the nation's foremost resources in the fields of child, adolescent, adult, and geriatric mental health. Together they constitute one of the largest departments in the UCSF School of Medicine and the UCSF Weill Institute for Neurosciences, with a mission focused on research (basic, translational, clinical), teaching, patient care, and public service.
UCSF Psychiatry and Behavioral Sciences conducts its clinical, educational, and research efforts at a variety of locations in Northern California, including the UCSF Nancy Friend Pritzker Psychiatry Building; UCSF Langley Porter Psychiatric Hospital; UCSF Medical Centers at Parnassus Heights, Mission Bay, and Mount Zion; UCSF Benioff Children’s Hospitals in San Francisco and Oakland; Zuckerberg San Francisco General Hospital and Trauma Center; the San Francisco VA Health Care System; UCSF Fresno; and numerous community-based sites around the San Francisco Bay Area.
About the UCSF Weill Institute for Neurosciences
The UCSF Weill Institute for Neurosciences, established by the extraordinary generosity of Joan and Sanford I. "Sandy" Weill, brings together world-class researchers with top-ranked physicians to solve some of the most complex challenges in the human brain.
The UCSF Weill Institute leverages UCSF’s unrivaled bench-to-bedside excellence in the neurosciences. It unites three UCSF departments—Psychiatry and Behavioral Sciences, Neurology, and Neurological Surgery—that are highly esteemed for both patient care and research, as well as the Neuroscience Graduate Program, a cross-disciplinary alliance of nearly 100 UCSF faculty members from 15 basic-science departments, as well as the UCSF Institute for Neurodegenerative Diseases, a multidisciplinary research center focused on finding effective treatments for Alzheimer’s disease, frontotemporal dementia, Parkinson’s disease, and other neurodegenerative disorders.
About UCSF
The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. UCSF Health, which serves as UCSF’s primary academic medical center, includes top-ranked specialty hospitals and other clinical programs, and has affiliations throughout the Bay Area.