UCSF emphasizes innovation and creativity, and the Adult Psychiatry Residency Training Program offers a clinical curriculum in which residents become expert clinicians and leaders in the field. The program provides broad exposure to a diversity of patients, modalities, therapies, and environments, while also highlighting longitudinal relationships with patients, faculty, and clinical systems.
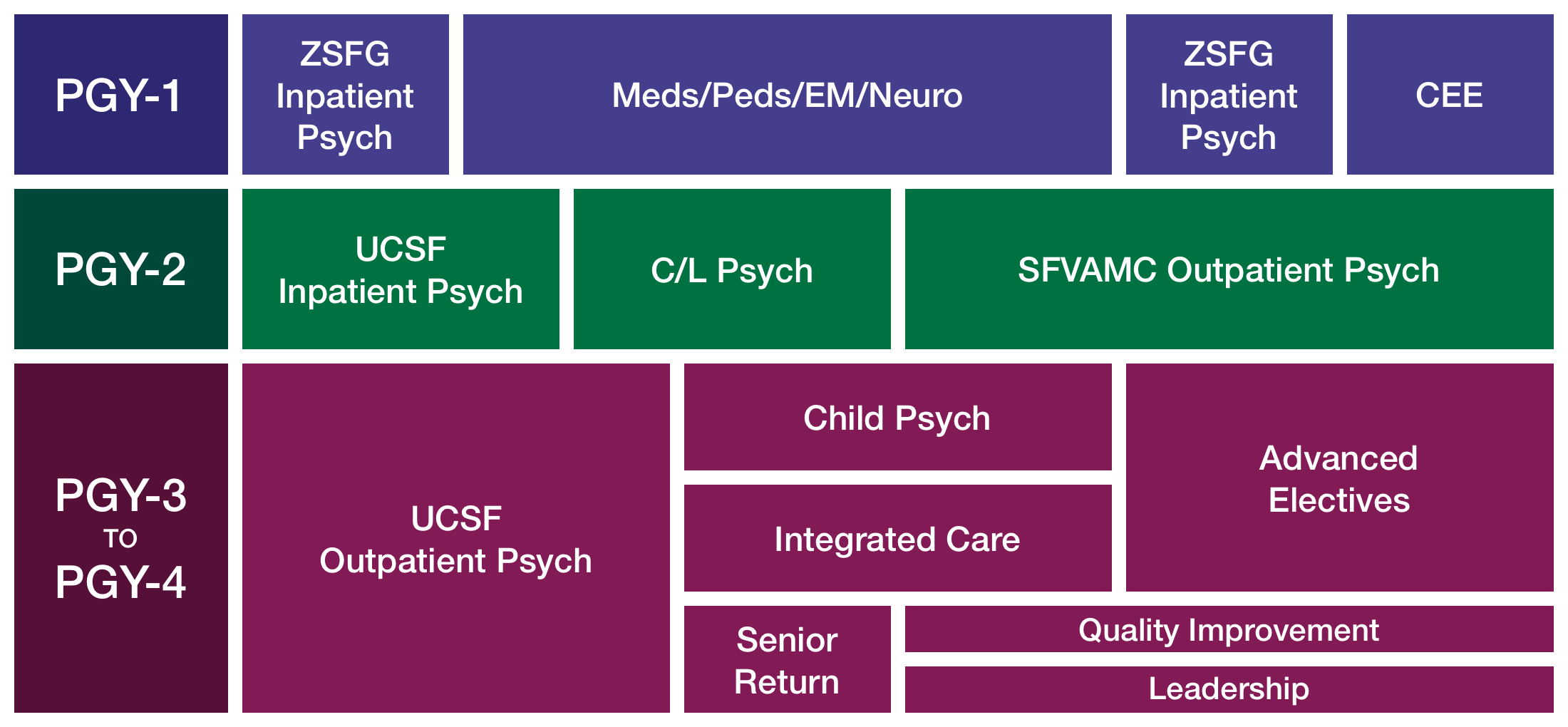
- PGY-1: Forging a New Identity as a Physician
- PGY-2: Developing Skills Across the Continuum of Care
- PGY-3: Honing Expertise Across the Lifespan
- PGY-4: Launching Leaders in Psychiatry
Longitudinal Clinical Experience (LCE)
The Longitudinal Clinical Experience (see Program Highlights for more detail) begins in the first year. Residents are assigned to a half-day clinic where they work in teams with faculty and resident peers (PGY-1 to PGY-4), providing assessment, pharmacotherapy, psychotherapy, and management of a cohort of patients in a specific population (e.g., women, geriatric, bipolar disorder, early psychosis, LGBTQ+, etc.) that they will follow throughout their four years of residency.
In the LCE, residents have the opportunity to receive feedback longitudinally from core faculty members who watch them develop diagnostic reasoning and clinical skills mastery across four years of training. Senior residents in each clinic provide near-peer mentorship and hone their leadership skills, supervising and teaching junior residents, assisting in clinic management, coordinating case conferences, and leading team meetings.
PGY-1: Forging a New Identity as a Physician
The intern year functions to consolidate core skills from medical school into a new identity as a physician and budding psychiatrist. Our PGY-1 interns complete core rotations in:
Medicine/neurology (6 months)
- Inpatient medicine (2 months)
- Outpatient medicine/urgent care (1 month)
- Emergency medicine (1 month)
- Inpatient neurology (1 month)
- Outpatient behavioral neurology (1 month)
These core experiences in internal medicine, neurology, and emergency medicine occur at the UCSF Medical Center at Mission Bay, Zuckerberg San Francisco General Hospital and Trauma Center (ZSFG), and San Francisco VA Medical Center (SFVAMC), all of which are shared training sites and experiences with colleagues in UCSF’s renowned internal medicine and neurology residency programs.
For those residents interested in a career in child and adolescent psychiatry, one of the months of inpatient medicine can be substituted with an experience in adolescent medicine and the month of inpatient neurology can be substituted with a rotation with the child neurology consultation service.
Outpatient neurology is spent at the world-renowned UCSF Memory and Aging Center, where the experience emphasizes the behavioral and neuropsychiatric aspects of neurological disorders including the work-up, diagnosis, and management of Alzheimer’s disease, chronic traumatic encephalopathy, frontotemporal dementia, HIV-related cognitive impairment, Huntington’s disease, Parkinson’s disease, and vascular dementia.
Public and community psychiatry (6 months)
- Inpatient public psychiatry at ZSFG (4 months)
- CEE: Clinical evaluations and emergency (2 months)
Four months of the PGY-1 year are spent learning the principles of inpatient psychiatric assessment and treatment at ZSFG, providing services to San Francisco’s medically and economically disadvantaged, and a population experiencing serious and persistent mental illness, under the supervision of core faculty with expertise in public and community psychiatry. Here residents will gain experience working with a diverse population of patients including those experiencing homelessness, who are uninsured, who are under public conservatorship, who have serious persistent illness, or might be experiencing first episode psychosis. Residents also spend time in the San Francisco County Jail’s inpatient psychiatry unit located at ZSFG, learning forensic psychiatry.
The clinical evaluations and emergency (CEE) rotation includes four weeks of emergency psychiatry at ZSFG, providing comprehensive emergency psychiatric services to patients experiencing acute mental health crises and assessments of suicide risk, violence risk, and criteria for civil commitment, and three weeks of exposure to outpatient psychiatric clinics and services across the health system with a focus on developing foundational skills in psychiatric diagnostic evaluation.
Clinics and services featured during CEE include a community buprenorphine induction clinic, an assertive outpatient treatment team at UCSF Citywide Case Management, electroconvulsive therapy and transcranial magnetic stimulation services at UCSF, specialty psychiatry services at UCSF—including the child Hyperactivity, Attention, and Learning Problems Clinics, the Tic, Anxiety and OCD Clinic, the LGBTQ Mental Health Clinic, consultation services such as psycho-oncology and women’s mental health, and community psychiatry at Chinatown North Beach.
PGY-2: Developing Skills Across the Continuum of Care
Skills gained during intern year are further developed in PGY-2, with core rotations across the continuum of care in psychiatry from rotations on acute inpatient wards, to consultation-liaison services to medical-surgical wards, labor and delivery, and intensive care units, and a six-month continuous experience in longitudinal experience in outpatient psychiatry, addiction care, and initial experiences in individual and couples psychotherapy.
Inpatient psychiatry at UCSF Langley Porter Psychiatric Hospital (3 months)
PGY-2 residents complete a three-month rotation on the adult psychiatry inpatient unit at UCSF Langley Porter Psychiatric Hospital (LPPH) at Mount Zion. Founded in 1941 as California’s first neuropsychiatric institute, LPPH consists of an adult inpatient unit, an adult partial hospitalization program, and an adult intensive outpatient program. The acute locked inpatient unit serves a broad patient population, with ages ranging from late teens to 90+, from all socioeconomic classes, and with a wide range of clinical presentations. There is also an active electroconvulsive therapy (ECT) service, and residents will refer and follow patients receiving ECT who may have emergent psychiatric needs and/or severe and treatment-resistant mental disorders.
Consultation-liaison psychiatry (3 months)
During the PGY-2 year, residents spend three months providing consultation-liaison services at either ZSFG or the UCSF Medical Center at Parnassus Heights, working closely with faculty to learn how to evaluate psychiatric manifestations of medical disorders and develop techniques to manage primary psychiatric disorders for patients who are medically hospitalized, in collaboration with other disciplines.
UCSF Medical Center is recognized throughout the world as the leader in health care, and is known for advanced technology, innovative medicine, and compassionate care and is consistently ranked as one of the nation’s top 10 hospitals according to U.S. News and World Report. Residents rotating with the UCSF Parnassus consultation-liaison service will provide comprehensive consultation and liaison services, in tandem with faculty experts in transplantation psychiatry, critical care psychiatry, reproductive psychiatry, neuropsychiatry, and psycho-oncology.
Zuckerberg San Francisco General Hospital and Trauma Center seeks to provide world-class care for all the people of San Francisco, regardless of ability to pay or immigration status. ZSFG serves as San Francisco and Northern San Mateo’s only Level 1 Trauma Center and the world’s leader in HIV/AIDS care. It is also home to 20 UCSF research centers, with research budgets exceeding $200 million annually. Residents rotating with the ZSFG consultation-liaison service will provide consultative services with attending psychiatrists with expertise in public and community psychiatry, traumatic brain injury, HIV/AIDS psychiatry, palliative care psychiatry, and LGBTQ psychiatry.
Outpatient clinics, addiction care, and psychotherapy (3 months)
Six months of PGY-2 year is spent in a full-time rotation at SFVAMC, designed to give residents early exposure to the principles of outpatient psychiatry evaluation and treatment. With close supervision in several settings, residents learn a variety of treatment modalities including comprehensive diagnostic evaluations, pharmacotherapy, and psychotherapy. All residents participate in clinics devoted to rapid evaluation, substance use disorders, psychopharmacology, and specialized PTSD treatment. Psychotherapy training includes individual therapy (interpersonal therapy and cognitive behavioral therapy), group therapy (substance use disorders and long-term process group), and couples/family therapy. Core experiences in addiction psychiatry through a trauma-informed lens, are provided in the SFVAMC rotation.
PGY-3: Honing Psychiatric Expertise Across the Lifespan
Specialty care clinics, medication management, and psychotherapy
The PGY-3 year is a largely outpatient experience located primarily at the UCSF Nancy Friend Pritzker Psychiatry Building near the UCSF Mission Bay campus. Residents provide a variety of psychiatric clinical services in this ambulatory care setting, including intake and assessment in specialty clinics, and longitudinal psychotherapy and medication management.
Specialty clinics are half-day clinics organized by diagnostic category or patient population and are designed to provide comprehensive teaching and “real-time” supervision. Clinics include depressive disorders, bipolar spectrum disorders, tic and obsessive-compulsive disorders, women’s mental health, early psychosis intervention, geriatric psychiatry, and LGBTQ+ mental health.
Special attention is given to the educational experience of residents in the outpatient clinics to provide expert training, supervision and support in the application of diverse treatment models, including pharmacotherapy, neuromodulation, and psychotherapy (e.g., supportive psychotherapy, cognitive behavioral therapy (CBT), interpersonal psychotherapy (IPT), psychodynamic psychotherapy, dialectic behavioral therapy (DBT), problem solving therapy (PST), and acceptance and commitment therapy (ACT)).
Integrated care rotation (ICR)
During the PGY-3 or PGY-4 year, residents serve as co-located clinicians and/or collaborative care consultants in an integrated care model, in settings such as primary care, obstetrics, oncology, HIV, and neurology. The experience is highly interdisciplinary, and residents have the opportunity to participate in team meetings and clinical encounters emphasizing sequenced and shared visits with other specialties, open access to mental health services, and warm hand-offs between specialty services.
Residents rotate for one half-day over the course of one academic year. Sites for this rotation include the ZSFG High Risk OB Service, UCSF Psychiatry-OB Clinic, UCSF Psychiatry-HIV Clinic, UCSF Psycho-Oncology Clinic, UCSF Movement Disorders Clinic, and the psychiatry-primary care clinics at SFVAMC and UCSF Mount Zion.
Child and adolescent psychiatry
PGY-3 residents also spend one half-day per week throughout the year in child and adolescent psychiatry, which consists of didactics and clinical experience observing and conducting supervised comprehensive psychiatric evaluations of children, adolescents, and families. In addition, residents do weekly outpatient therapy with a child or adolescent and participate in weekly individual supervision about their case. Seminars teach residents about normal child development, therapy, and childhood psychopathology. Electives in the Tourette’s and Pervasive Development Disorders (Autism) Clinic are also available.
Training sites include the UCSF Nancy Friend Pritzker Psychiatry Building, San Francisco Department of Public Health Community Behavioral Health Clinics (e.g., Chinatown Development Center), and UCSF Benioff Children's Hospital Oakland.
Quality improvement
In the PGY-3 year, every resident is provided with four one-week blocks of protected time to lead a quality improvement effort. Each resident is paired with a QI faculty mentor to help in project development, implementation, and evaluation. Quality improvement projects may be based at any of our core rotation sites. At the end of the academic year, all PGY-3 residents present their QI work at a symposium for Department of Psychiatry and Behavioral Sciences faculty and residents
PGY-4: Launching Leaders in Psychiatry: In Clinical Care, Research, Education, and Public Policy
Longitudinal medication management and psychotherapy clinics
Emphasis on longitudinal care continues into the PGY-4 year, where residents carry medication management and psychotherapy cases over from the PGY-3 year.
Advanced electives
A majority of the PGY-4 year is elective and is designed to ensure that the experiences residents select have a coherent theme. These experiences aim to advance professional development by promoting growth as a leader, an educator, an expert in a specific area, and an outstanding clinician.
During the second half of the PGY-3 year, residents (with support from advisors and mentors) develop personalized learning goals for their fourth year and then construct an individualized set of elective experiences to meet those goals. Residents choose from a variety of senior resident rotations across all of UCSF’s training sites, drawing from several broad areas of concentration (e.g., community and public psychiatry, outpatient psychotherapy, pharmacotherapy, inpatient care, consultation/liaison, interventional psychiatry, etc.).
In both the PGY-3 and PGY-4 years, residents also have the opportunity for up to one half day of protected scholarship time to work on their residency scholarly project or pursue other areas of interest with a dedicated mentor. At the end of fourth year, each resident presents a Senior Talk on their residency scholarly project to the department.
The Research Resident Training Program (RRTP) recruits trainees who are clear in their goal to pursue a research career post-residency, which typically entails several years of a postdoctoral research fellowship. RRTP provides active mentorship and support in helping residents become physician-scientists in basic science, translational, clinical, and health services research. Residents in this program have scheduled time devoted specifically to research: up to 5% in the PGY-1 year, up to 20% in the PGY-2 year, up to 35% in the PGY-3 year, and up to 90% in the PGY-4 year.
The training program also encourages motivated residents to fast-track into the UCSF Public Psychiatry Fellowship, in which they work three days a week in a community mental health clinic, attend the same didactics as the PGY-5 Public Psychiatry Fellows, and complete a rigorous program evaluation/quality improvement project by developing a public-academic partnership. Residents continue to satisfy core general psychiatry residency program requirements and complete their fellowship by the conclusion of their PGY-4 year.
Leadership and “Senior Return” Month
Residents are expected to develop leadership skills during residency and to be effective agents of change in health care systems. Our leadership curriculum reflects this vision of creating future leaders in the field, with an emphasis on understanding one’s leadership personality and styles and team and group process. At the end of training, residents will have led one or more systems improvement/QI projects, served as members on important residency training, department, School of Medicine, or university committees; participated as a team leader in a variety of clinical settings, including intensive services and ambulatory care services; and participated in the PGY-4 leadership and career development seminars.
Residents complete a required, immersive “Senior Return Month” (aka “Junior Attending Month”) on a consultation/liaison or inpatient service. Across all senior rotations, residents assume leadership roles in the administrative and educational processes of the rotations, functioning, for example, as team leaders and teachers to junior residents.
Chief Residents, Resident Champions, and the Residents Association
The program has several resident leadership roles. There are seven Chief Resident positions, including four site-based Chief Residents (UCSF Intensive Services, Pritzker Outpatient Services, ZSFG, and SFVAMC), a Community Programs Chief Resident, an Education Chief Resident, and a Research Chief Resident. These residents receive special opportunities to develop teaching, leadership, and administrative skills and play crucial roles in all aspects of the training program. Chiefs are selected by the Residency Training Program faculty, with input from service chiefs. They meet weekly with the program director as a group and also individually with the site director at their respective sites.
In addition to chief residents, there are positions for Resident Champions to support resident well-being and equity, inclusion, and belonging. There are also elected leadership positions in the Residents Association (RA), which is composed of all UCSF Adult Psychiatry Residency Training Program residents. The RA leadership meets weekly with all residents, serves as representatives on residency governance committees, offers teaching awards to faculty educators, plans the annual resident retreat, and plans the end-of-year residency gala celebration.